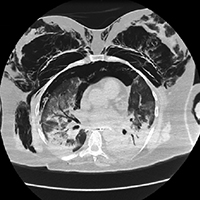
Pneumothorax and pneumomediastinum in COVID-19 acute respiratory distress syndrome
Submitted: September 15, 2020
Accepted: March 6, 2021
Published: April 16, 2021
Accepted: March 6, 2021
Abstract Views: 3072
PDF: 1436
VIDEO: 186
VIDEO: 186
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Massimiliano Polastri, Lara Pisani, Andrea Dell'Amore, Stefano Nava, Revolving door respiratory patients: A rehabilitative perspective , Monaldi Archives for Chest Disease: Vol. 87 No. 3 (2017)
- S. Bertini, M. Picariello, M. Gorini, T. Renda, A. Augustynen, G. Villella, G. Misuri, N.M. Maluccio, R. Ginanni, D. Tozzi, A. Corrado, Telemonitoring in chronic ventilatory failure: a new model of survellaince, a pilot study , Monaldi Archives for Chest Disease: Vol. 77 No. 2 (2012): Pulmonary series
- Gianfranco Beghi, Antonio De Tanti, Paolo Serafini, Chiara Bertolino, Antonietta Celentano, Graziella Taormina, Monitoring of hospital acquired pneumonia in patients with severe brain injury on first access to intensive neurological rehabilitation: First year of observation , Monaldi Archives for Chest Disease: Vol. 88 No. 1 (2018)
- Stefano Fumagalli, Serena Boni, Simone Pupo, Marta Migliorini, Irene Marozzi, Eleonora Barghini, Flavia Sacco, Niccolò Marchionni, Rate-control vs rhythm-control of atrial fibrillation in elderly patients. From new, age-oriented outcomes to a more complex management strategy , Monaldi Archives for Chest Disease: Vol. 88 No. 2 (2018)
- Samuele Baldasseroni, Francesco Orso, Alessandra Pratesi, Alice Foschini, Andrea Giosafat Marella, Nadia Bartoli, Ilaria Bracali, Alessando Antenore, Francesca Tarantini, Costanza Burgisser, Niccolò Marchionni, The complexity of risk stratification in older patient candidate to non-cardiac surgery , Monaldi Archives for Chest Disease: Vol. 78 No. 3 (2012): Cardiac series
- F. Novelli, F. Costa, M. Latorre, L. Malagrinò, A. Celi, B. Vagaggini, P. Paggiaro, Tiotropium: a new therapeutic option in asthma , Monaldi Archives for Chest Disease: Vol. 79 No. 3-4 (2013): Pulmonary series
- A. Chroneou, N. Zias, A.V. Gonzalez, J.F. Beamis Jr, Tracheobronchopathia Osteochondroplastica. An underrecognized entity? , Monaldi Archives for Chest Disease: Vol. 69 No. 2 (2008): Pulmonary series
- Stefano Romagnoli, Laura Paparella, Paolo Boninsegni, The criteria of “inoperability†, Monaldi Archives for Chest Disease: Vol. 87 No. 2 (2017)
- M. Vitacca, J. Escarrabill, G. Galavotti, A. Vianello, E. Prats, R. Scala, A. Peratoner, E. Guffanti, L. Maggi, L. Barbano, B. Balbi, Home mechanical ventilation patients: a retrospective survey to identify level of burden in real life , Monaldi Archives for Chest Disease: Vol. 67 No. 3 (2007): Pulmonary series
- Zeynep Çınar, Eda Macit Aydın, Nurgul Naurzvai, Ayshan Mammadova, Sümeyye Kodalak, Aygül Abbasova, Gül Gürsel, Impact of neurological problems on mechanical ventilation and intensive care unit outcomes in pulmonary intensive care unit patients: a retrospective analysis of a single-center cohort , Monaldi Archives for Chest Disease: Vol. 94 No. 1 (2024)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/monaldi.2021.1608
https://doi.org/10.4081/monaldi.2021.1608





