Factors associated with time to sputum culture conversion of rifampicin-resistant tuberculosis patients in Klaipeda, Lithuania in 2016-2019: a cohort study
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
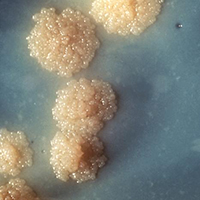
The global proportion of successful treatment outcomes of Multidrug-Resistant/Rifampicin-Resistant Tuberculosis (MDR/RR-TB) remains unacceptably low. Time to culture conversion is important in making treatment-related decisions and is used as an interim predictor of pulmonary MDR/RR-TB treatment success. No previous studies have been conducted to assess determinants of time to culture conversion for MDR/RR-TB patients in Lithuania. Secondary analysis of data of culture-positive MDR/RR-TB patients, treated in Republican Klaipeda Hospital between 1st July 2016 and 1st July 2019 was performed. Culture conversion was defined as two consecutive negative cultures on solid media submitted at least 30 days apart. Factors associated with culture conversion were estimated by crude and multivariable Cox regression accounting for competing risks. In total, 115 consecutive patients starting treatment were included in the study. Of them, the majority was male (86/115; 74.8%) with a mean age of 48 (standard deviation (SD) ±12) years and Human Immunodeficiency Virus (HIV) negative (105/115; 91.3%). Nearly two-thirds (72/115; 62.6%) had XDR (extensive drug resistance) or MDR/RR-TB with additional resistance to second-line injectables or fluoroquinolones. Of 115 culture-positive patients at baseline, 103 (89.6%) patients achieved culture conversion during 12 months of treatment. The median time to culture conversion was 1.1 months (interquartile range: 0.9-1.8). Patients aged ≥60 years compared with <40 years [adjusted hazard ration (aHR): 0.40, 95% confidence interval (CI): 0.18-0.86], smokers (aHR: 0.39, 95% CI: 0.2-0.73), patients with positive sputum smear microscopy at baseline (aHR: 0.40, 95% CI: 0.25-0.63), cavities on initial chest X-ray (aHR: 0.56, 95% CI: 0.35-0.88) and resistance to at least one fluoroquinolone drug (aHR: 0.52, 95% CI: 0.32-0.84) were slower to culture convert. In conclusion, we recommend providing additional counseling, treatment adherence interventions and scale up the use of new and repurposed TB drugs to patient groups at risk of worse interim treatment outcome: patients aged 60 and above, with resistance to fluoroquinolones, smear–positive, smokers, or with signs of extensive disease evident on initial chest radiography.






