Anabolic hormones and heart failure with preserved ejection fraction: looking for Ariadne’s thread
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
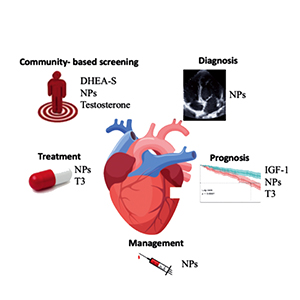
Heart failure with preserved ejection fraction (HFpEF) is a complex clinical syndrome that accounts for more than half of all heart failure patients. Identification, early diagnosis and management of patients are still complex, and no targeted treatment is available, since all tested drugs were not able to lower hard clinical outcomes. A multi-hormonal deficiency syndrome has been described in HFpEF patients suggesting that different hormones may represent new biomarkers of the disease, but their clinical utility is still debated. The natriuretic peptides are the cornerstone biomarker in heart failure, predicting cardiovascular death and heart failure hospitalization. Testosterone and DHEA-S deficiencies have been reported in HFpEF and associated with right ventricular impairment and diastolic dysfunction. IGFBP-1/IGF-1 axis correlates with echocardiographic parameters of HFpEF patients and with several prognostic biomarkers including NT-proBNP and C reactive protein. Low triiodothyronine syndrome is frequently found in HFpEF and thyroid hormones should represent a potential biomarker of risk stratification and prognosis.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






