Gender differences in the detection of carotid atherosclerosis: DUPLEX registry cross-sectional study results
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
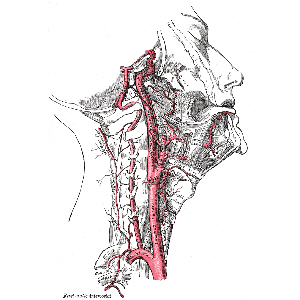
The aim of this study was to assess the features of detecting carotid atherosclerosis depending on gender, age, the presence of arterial hypertension, other major diseases and conditions according to The Duplex Registry Database. The registry sequentially included the results of duplex scanning of the carotid arteries (DSCA) of all patients who underwent it at the United Hospital with Outpatient Department in 2013 (n=2548). The incidence of carotid atherosclerosis (CAS) was higher in men than in women (58.6% (n=763) vs 45.5% (n=568), p<0.0000001). This was noted in all categories according to the gradation of stenosis, including in the category of the most severe lesion (>70%): 2.9% (n=32) vs 1.0% (n=13), p=0.003. The presence of CAD significantly increased the chances of detecting CAS in men (OR 4.47 vs 2.6, p<0.0000001). Signs more significant in their influence in women compared to men were the following: age (OR 5.3 [4.12; 6.71] p<0.0000001); arterial hypertension (OR 2.7 [2.12; 3.39] p<0.0000001) and cerebrovascular disease (OR 1.63 [1.13; 2.36] p=0.004). The OR of CAS detection for the “acute cerebrovascular accident” diagnosis in men and women differed 2 times (OR 1.2, p=0.4 vs 2.4, p=0.15). The “hypercholesterolemia” diagnosis when referred for DSCA did not show itself as a predictor of CAS detection in all study groups. Disorders of autonomic nervous system, hearing loss and screening examination showed a significant decrease in the probability of CAS detecting for the whole group (OR 0.14 [0.08;0.24] p<0.0000001; OR 0.16 [0.02;0.66] p=0.004 and OR 0.3 [0.25 0.37] p<0.0000001, respectively), so and separately for males and females. The present study revealed significant gender differences in the prevalence of carotid atherosclerosis and in the influence of various signs on an increase in the chances of its detection. The most significant signs were (OR men vs women): gender (1.3 vs 0.8), age (4.2 vs 5.3), arterial hypertension (1.8 vs 2.7), CAD (4.4 vs 2.6), cerebrovascular disease (1.26 vs 1.63).
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.







