Efficacy of a rehabilitation protocol on pulmonary and respiratory muscle function and ultrasound evaluation of diaphragm and quadriceps femoris in patients with post-COVID-19 syndrome: a series of cases
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
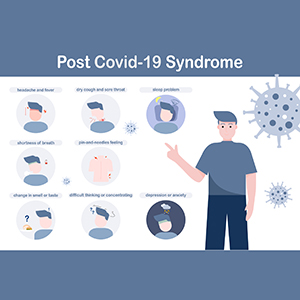
This study assessed the efficacy of a pulmonary rehabilitation (PR) on pulmonary and respiratory muscle function and thickness of quadriceps femoris and diaphragm of patients with post-COVID-19 syndrome. This series of cases followed nine patients who performed PR twice a week for six weeks. Patients received the following PR program: lung expansion therapy; respiratory muscle training; upper limb strength exercises; aerobic exercises on a treadmill. After the program, we observed increased peak expiratory flow (26.03%), forced vital capacity (FVC) (7.14%), forced expiratory volume in the first second (FEV1) (9.55%), and ratio between FEV1/FVC (6.19%). All parameters of respiratory muscle strength and endurance were improved. Diaphragmatic thickening fraction and thickness of quadriceps femoris also improved, whereas echo intensity of quadriceps reduced. Thus, RP protocol improved pulmonary function, respiratory muscle strength and endurance, and thickness of diaphragm and quadriceps femoris, and reduced echo intensity of quadriceps in patients with post-COVID-19 syndrome.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






