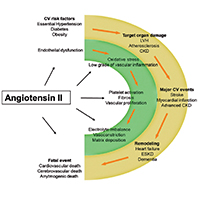
Effects of inhibition of the renin-angiotensin system on hypertension-induced target organ damage: clinical and experimental evidence
Submitted: August 13, 2020
Accepted: October 3, 2020
Published: February 10, 2021
Accepted: October 3, 2020
Abstract Views: 1104
PDF: 744
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Manoj Kumar, Rajesh Kumar Gupta, Raj Kumar, Sonam Spalgais, Anil Kumar Mavi, Kamal Singh, Cockroach exposure and its allergy sensitization in asthma patients , Monaldi Archives for Chest Disease: Vol. 91 No. 3 (2021)
- Christos Michailides, Dimitrios Velissaris, Common anti-oxidant vitamin C as an anti-infective agent with remedial role on SARS-CoV-2 infection. An update , Monaldi Archives for Chest Disease: Vol. 91 No. 4 (2021)
- Giorgio E. Polistina, Camilla Di Somma, Martina Flora, Alberto E. Maraolo, Novella Carannante, Gerardo Langella, Angela I. Mirizzi, Anna Annunziata, Giuseppe Fiorentino, Respiratory Intensive Care Unit management and efficacy during the COVID-19 outbreak in Naples, Italy , Monaldi Archives for Chest Disease: Vol. 93 No. 2 (2023)
- Shayan Shahid, Ali bin Abdul Jabbar, Abdullah Wagley, Muhammad Daniyal Musharraf, Haris Zahid, Syed Muhammad Zubair, Muhammad Irfan, Non-cystic fibrosis bronchiectasis: a retrospective review of clinical, radiological, microbiological and lung function profile at a tertiary care center of low-middle income country , Monaldi Archives for Chest Disease: Early Access
- Mamta Singh, Kunal Deokar, Bibhuti Prassan Sinha, Jinish Doshi, CDS Katoch, Infective pulmonary diseases and the eye: a narrative review , Monaldi Archives for Chest Disease: Early Access
- Carlo Iadevaia, Fabio Perrotta, Grazia Mazzeo, Francesco Saverio Cerqua, Gennaro Mazzarella, Salvatore Guarino, Roberto Parrella, Andrea Bianco, Incidental diagnosis of lung adenocarcinoma following coronavirus OC 43 severe pneumonia , Monaldi Archives for Chest Disease: Vol. 90 No. 3 (2020)
- Cinzia Nugara, Annamaria Lo Voi , Davide Diana, Silvia Sarullo, Antonino Zarcone, Filippo M. Sarullo, A case of extensive biatrial clot straddling the patent foramen ovale , Monaldi Archives for Chest Disease: Vol. 91 No. 2 (2021)
- Emrah Doğan, Utku Tapan, Özge Oral Tapan, Fatih Alaşan, Sabri Serhan Olcay, Tuğba Çınar Olcay, A case of B.1.1.7 SARS-CoV-2 UK strain with an atypical radiological presentation , Monaldi Archives for Chest Disease: Vol. 91 No. 4 (2021)
- Alberto Fantin, Nadia Castaldo, Paolo Vailati, Giuseppe Morana, Vincenzo Patruno, Full medical treatment of COVID-19 associated large pneumothorax - A case report , Monaldi Archives for Chest Disease: Vol. 92 No. 1 (2022)
- Bhaskar Kakarla, Bronchocele, a common but underrecognized condition: a systematic review , Monaldi Archives for Chest Disease: Vol. 93 No. 1 (2023)
<< < 79 80 81 82 83 84 85 86 87 88 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/monaldi.2021.1570
https://doi.org/10.4081/monaldi.2021.1570




