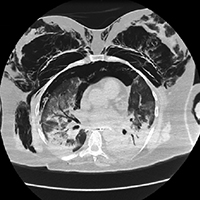
Pneumothorax and pneumomediastinum in COVID-19 acute respiratory distress syndrome
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 6 March 2021
Authors
COVID-19 has involved numerous countries across the globe and the disease burden, susceptible age group; mortality rate has been variable depending on the demographical profile, economic status, and health care infrastructure. In the current clinical environment, COVID-19 is one of the most important clinical differential diagnoses in patients presenting with respiratory symptoms. The optimal mechanical ventilation strategy for these patients has been a constant topic of discussion and very importantly so, since a great majority of these patients require invasive mechanical ventilation and often for an extended period of time. In this report we highlight our experience with a COVID-19 patient who most likely suffered barotrauma either as a result of traumatic endotracheal intubation or primarily due to COVID-19 itself. We also aim to highlight the current literature available to suggest the management strategy for these patients for a favorable outcome. The cases described are diverse in terms of age variance and other comorbidities. According to the literature, certain patients, with COVID-19 disease and spontaneous pneumothorax were noted to be managed conservatively and oxygen supplementation with nasal cannula sufficed. Decision regarding need and escalation to invasive mechanical ventilation should be taken early in the disease to avoid complications such as patient self-inflicted lung injury (P-SILI) and barotrauma sequelae such as pneumothorax and pneumomediastinum Recent systematic review further supports the fact that the use of non-invasive ventilation (NIV) in certain patients with COVID-19 pneumonia may give a false sense of security and clinical stabilization but has no overall benefit to avoid intubation. While invasive mechanical ventilation may be associated with higher rates of barotrauma, this should not mean that intubation and invasive mechanical ventilation should be delayed. This becomes an important consideration when non-intensivists or personnel with less experience provide care for this vulnerable patient population who may rely too heavily on NIV to avoid intubation and mechanical ventilation.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






