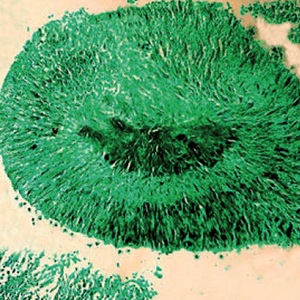
Pulmonary actinomycosis: cytomorphological features
Submitted: October 15, 2020
Accepted: September 22, 2021
Published: November 5, 2021
Accepted: September 22, 2021
Abstract Views: 1363
PDF: 750
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Debapriya Maji, Upasna Agarwal, Lokender Kumar, Vinay V, Amit Sharma, Clinicodemographic profile and outcome of tuberculosis treatment in TB-HIV co-infected patients receiving daily ATT under a single window TB-HIV services delivery initiative , Monaldi Archives for Chest Disease: Vol. 93 No. 3 (2023)
- Emmanouil Panagiotou, Ioannis Vamvakaris, Nikolaos K. Syrigos, Elias Kotteas, Pulmonary benign metastasizing leiomyoma: a case report , Monaldi Archives for Chest Disease: Vol. 94 No. 1 (2024)
- Angelica Cersosimo, Mauro Riccardi, Ludovica Amore, Giuliana Cimino, Gianmarco Arabia, Marco Metra, Enrico Vizzardi, Varicella zoster virus and cardiovascular diseases , Monaldi Archives for Chest Disease: Vol. 93 No. 2 (2023)
- Nabila Kanwal, Humza Thobani, Ainan Arshad, Priya Ashok Kumar, Fatima Amjad, Safia Awan, Muhammad Irfan, Factors predicting mortality among patients with COVID-19 associated hospital acquired pneumonia: insights from a tertiary care center , Monaldi Archives for Chest Disease: Vol. 93 No. 4 (2023)
- Devika Tayal, Prerna Jain, Mamta Bhardwaj, Amit Sharma, Diabetes mellitus in acute exacerbation of chronic obstructive pulmonary disease – the tip of the iceberg , Monaldi Archives for Chest Disease: Early Access
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/monaldi.2021.1641
https://doi.org/10.4081/monaldi.2021.1641





