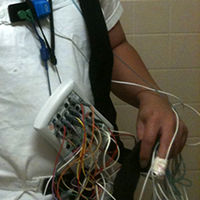
Role of esophageal manometry in polysomnography of patients with chronic respiratory failure
Submitted: December 29, 2020
Accepted: May 15, 2021
Published: July 22, 2021
Accepted: May 15, 2021
Abstract Views: 4584
PDF: 576
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Maral Ranjbar, Mojdeh Matloubi, Shaghayegh Sadegh, Morteza Fallahpour, Leila Janani, Mohammad-Ali Assarehzadegan, IL1RL1 single nucleotide polymorphisms are associated with asthma in the Iranian population , Monaldi Archives for Chest Disease: Vol. 92 No. 3 (2022)
- Brandon Iturbe Esquivel, José Meneses Calderón, Luis Edgar Concepción Carrillo, Hugo Mendieta Zeron, Rural treatment of COVID-19 patients with pirfenidone, nitazoxanide and colchicine. Case series , Monaldi Archives for Chest Disease: Vol. 93 No. 1 (2023)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/monaldi.2021.1756
https://doi.org/10.4081/monaldi.2021.1756





