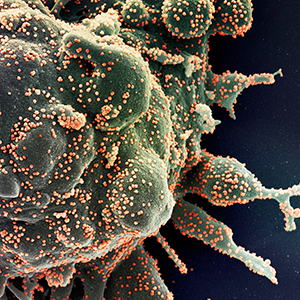
To study heterogeneity in SARS-CoV-2 IgG response titre in patients recovered from COVID-19
Published: September 28, 2021
Abstract Views: 1389
PDF: 511
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Amrutha S, Komaldeep Kaur, Deepak Aggarwal, Mandeep Kaur Sodhi, Shivani Jaswal, Varinder Saini, Serial evaluation of antibody titres in patients recovered from COVID-19 and their correlation with disease severity , Monaldi Archives for Chest Disease: Vol. 94 No. 4 (2024)
- Gian Francesco Mureddu, Current multivariate risk scores in patients undergoing non-cardiac surgery , Monaldi Archives for Chest Disease: Vol. 87 No. 2 (2017)
- M. Lusuardi, C. Lucioni, F. De Benedetto, S. Mazzi, C.M. Sanguinetti, C.F. Donner, GOLD severity stratification and risk of hospitalisation for COPD exacerbations , Monaldi Archives for Chest Disease: Vol. 69 No. 4 (2008): Pulmonary series
- Branko Beronja, Aleksandra Karan, Biljana Lukic, Ivana Milosevic, Jelena Dotlic, Tatjana Gazibara, Smoking patterns and outcomes of severe sars-CoV-2 infection: a retrospective cohort study , Monaldi Archives for Chest Disease: Early Access
- Neeta Singla, Amitesh Gupta, U.K. Khalid, Ravindra Kumar Dewan, Rupak Singla, Clinical profile, risk factors, disease severity, and outcome for COVID-19 disease in patients with tuberculosis on treatment under the National Tuberculosis Elimination Program: a cohort of 1400 patients , Monaldi Archives for Chest Disease: Early Access
- Maria Teresa La Rovere, Egidio Traversi, Prognostic impact of digoxin use for rate control of atrial fibrillation in patients ≥75 years of age , Monaldi Archives for Chest Disease: Vol. 88 No. 2 (2018)
- Vittorio Palmieri, Antonio Palermo, Patients’ self-evaluation of symptoms, signs and compliance to therapy for heart failure surveillance: A pilot study on identification of worsening heart failure , Monaldi Archives for Chest Disease: Vol. 88 No. 2 (2018)
- Abhishekl Agarwal, Sakshi Batra, Rajendra Prasad, Anand Verma, Abdul Q. Jilani, Surya Kant, A study on the prevalence of depression and the severity of depression in patients of chronic obstructive pulmonary disease in a semi-urban Indian population , Monaldi Archives for Chest Disease: Vol. 88 No. 1 (2018)
- Abhijeet Singh, Rajendra Prasad, Rajiv Garg, Surya Kant, Giridhar B. Hosmane, Abhisek Dubey, Abhisek Agarwal, Ram Kishun Verma, A study to estimate prevalence and risk factors of Obstructive Sleep Apnoea Syndrome in a semi-urban Indian population , Monaldi Archives for Chest Disease: Vol. 87 No. 1 (2017)
- Alice Biffi, Giulia Dei, Federica De Giacomi, Anna Stainer, Lorenzo Olmo Parma, Maria Rosa Pozzi, Paola Faverio, Alberto Pesci, Non-specific interstitial pneumonia and features of connective tissue disease: What are the consequences of a different point of view? , Monaldi Archives for Chest Disease: Vol. 88 No. 3 (2018)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/monaldi.2021.1943
https://doi.org/10.4081/monaldi.2021.1943





