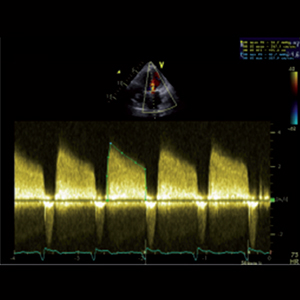
Loss of engagement in controlling chronic anticoagulation therapy during Covid-19 stringency measures. A single center experience of disproportioned increase of stuck mechanical valves
Submitted: August 25, 2021
Accepted: September 22, 2021
Published: December 3, 2021
Accepted: September 22, 2021
Abstract Views: 1024
PDF: 459
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- S. Dragonieri, O. Tongoussouva, A. Zanini, A. Imperatori, A. Spanevello, Markers of airway inflammation in pulmonary diseases assessed by induced sputum , Monaldi Archives for Chest Disease: Vol. 71 No. 3 (2009): Pulmonary series
- Giuseppe Francavilla, Maurizio Giuseppe Abrignani, Annabella Braschi, Rosalba Sciacca, Vincenzo Christian Francavilla, Marco Malvezzi Caracciolo, Nicola Renda, Carmine Riccio, Anna Scaglione, Giambattista Braschi, Physical exercise and Sport activities in patients with and without coronary heart disease , Monaldi Archives for Chest Disease: Vol. 68 No. 2 (2007): Cardiac series
- Michele Vitacca, Beatrice Salvi, Marta Lazzeri, Elisabetta Zampogna, Giancarlo Piaggi, Piero Ceriana, Serena Cirio, Luigino Rizzello, Grazia Lacala, Angelo Longoni, Vittoria Galimberti, Patrizia D'Ambrosio, Enrica Pavesi, Giuseppe La Piana, Antonella Sanniti, Alessandro Morandi, Manoel Vallet, Mara Paneroni, Respiratory rehabilitation for patients with COVID-19 infection and chronic respiratory failure: a real-life retrospective study by a Lombard network , Monaldi Archives for Chest Disease: Vol. 92 No. 3 (2022)
- D. Gorecka, J. Zieliński, Screening for chronic respiratory diseases in Georgia , Monaldi Archives for Chest Disease: Vol. 71 No. 4 (2009): Pulmonary series
- E. Vizzardi, S. Nodari, C. Fiorina, M. Metra, L. Dei Cas, Raised homocystein plasma concentration in patients with Heart Failure: clinical significance , Monaldi Archives for Chest Disease: Vol. 68 No. 2 (2007): Cardiac series
- Manu Dogra, Surabhi Jaggi, Deepak Aggarwal, Seema Gupta, Varinder Saini, Jasbinder Kaur, Role of interleukin-6 and insulin resistance as screening markers for metabolic syndrome in patients of chronic obstructive pulmonary disease. A hospital-based cross-sectional study , Monaldi Archives for Chest Disease: Vol. 92 No. 3 (2022)
- Alessandra Gualco, Cristina Opasich, Silvia Brazzo, Franco Cobelli, Evasio Pasini, Ornella Pastoris, Roberto Aquilani, Metabolic frailty in malnourished heart failure patients , Monaldi Archives for Chest Disease: Vol. 68 No. 2 (2007): Cardiac series
- Enrico Vizzardi, Pompilio Faggiano, Ermanna Chiari, Diego Maffeo, Silvia Frattini, Francesca Bellandi, Savina Nodari, Livio Dei Cas, The study of left ventricular diastolic function by Doppler echocardiography: the essential for the clinician , Monaldi Archives for Chest Disease: Vol. 72 No. 1 (2009): Cardiac series
- Alberto Genovesi Ebert, Furio Colivicchi, Marco Malvezzi Caracciolo, Carmine Riccio, Additive beneficial effects of beta blockers in the prevention of symptomatic heart failure , Monaldi Archives for Chest Disease: Vol. 72 No. 1 (2009): Cardiac series
- Fabiola B. Sozzi, Laura Iacuzio, Marta Belmonte, Marco Schiavone, Francesca Bursi, Elisa Gherbesi, Frank Levy, Ciro Canetta, Stefano Carugo, Early diagnosis of cardiomyopathies by cardiac magnetic resonance. Overview of the main criteria , Monaldi Archives for Chest Disease: Vol. 92 No. 4 (2022)
<< < 31 32 33 34 35 36 37 38 39 40 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/monaldi.2021.2065
https://doi.org/10.4081/monaldi.2021.2065





