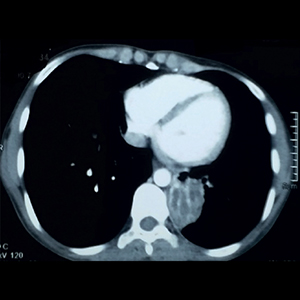
Bronchocele, a common but underrecognized condition: a systematic review
Submitted: November 26, 2021
Accepted: April 13, 2022
Published: April 22, 2022
Accepted: April 13, 2022
Abstract Views: 4676
PDF: 671
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Abhishek B J, Agadi Hiremath Viswanatha Swamy, Sanatkumar Bharamu Nyamagoud, Anupama George, Namratha D, Respiratory syncytial virus: an overview of clinical manifestations and management in the Indian pediatric population , Monaldi Archives for Chest Disease: Early Access
- Yogesh Kumar Jain, Pankaj Bhardwaj, Nitin Kumar Joshi, Manoj Kumar Gupta, Akhil Dhanesh Goel, Prem Prakash Sharma, Willingness to pay for a tobacco-free life: a contingent valuation assessment , Monaldi Archives for Chest Disease: Early Access
- Sonam Spalgais, Siddharth Raj Yadav, Parul Mrigpuri, Raj Kumar, Spirometry findings of chronic lung disease in high-altitude residents of Ladakh (>11,000 feet above sea level) , Monaldi Archives for Chest Disease: Early Access
- Maryam Hassan, Akbar Shoukat Ali, Ali Bin Sarwar Zubairi, Zahra Ali Padhani, Salman Kirmani, Huzaifa Ahmad, Zafar Fatmi, Jai K Das, Gene polymorphisms and risk of idiopathic pulmonary fibrosis: a systematic review and meta-analysis , Monaldi Archives for Chest Disease: Early Access
- Megha Hegde, Saurav Raj, Aishwarya S Pattanshetti, Sanatkumar Bharamu Nyamagoud, Gaining insights into chronic obstructive pulmonary disease exacerbation through emerging biomarkers and the chronic obstructive pulmonary disease assessment test score , Monaldi Archives for Chest Disease: Early Access
- Manju Bala, Akhlesh Rajpoot, Dinesh Chandra Punera, Suyash Singh Rathore, Hormonal harmony disrupted: hypothyroidism and diabetes mellitus in interstitial lung disease. An observational study , Monaldi Archives for Chest Disease: Early Access
- Marcos Martinelli, Eduardo V. Ponte, Daniel Antunes S. Pereira, Giulio Checchinato , Bruna Eduarda Gandra, Bruno Maciel, Alcides Rocha, Relationship between symptoms and results on spirometry in adults seen in non-tertiary public health facilities presenting with preserved ratio impaired spirometry , Monaldi Archives for Chest Disease: Early Access
- Mamta Singh, Kunal Deokar, Bibhuti Prassan Sinha, Jinish Doshi, CDS Katoch, Infective pulmonary diseases and the eye: a narrative review , Monaldi Archives for Chest Disease: Early Access
- Raj Kumar, Manoj Kumar, Sukriti Raj, Rachna Rachna, Jyoti Mishra, Shyam Mani Dubey, Sourav Kumar, Dileep Kumar Arisham, Gunjan Goutam, Anil Kumar Mavi, Quitting tobacco through quitline services: impact in India , Monaldi Archives for Chest Disease: Early Access
- Paola Gnerre, Ombretta Para, Dino Stefano Di Massimo, Tiziana Marcella Attardo, Dario Manfellotto, Francesco Dentali, Prevalence, risk factors and clinical impact of burnout in internal medicine units: a call to action , Monaldi Archives for Chest Disease: Early Access
<< < 15 16 17 18 19 20 21 22 23 24 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/monaldi.2022.2133
https://doi.org/10.4081/monaldi.2022.2133





