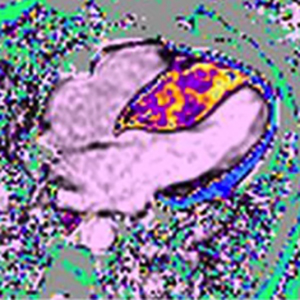
Early diagnosis of cardiomyopathies by cardiac magnetic resonance. Overview of the main criteria
Submitted: February 28, 2022
Accepted: March 15, 2022
Published: April 11, 2022
Accepted: March 15, 2022
Abstract Views: 1279
PDF: 540
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- G. Buccheri, D. Ferrigno, M.C. Giordano, Weekly chemotherapy with cisplatin and paclitaxel in advanced NSCLC: a phase II study , Monaldi Archives for Chest Disease: Vol. 65 No. 2 (2006): Pulmonary series
- Sh. Karimi, F. Mohammadi, S. Pejhan, M. Bakhshayeshkaram, P. Akhavan-Azari, M. Bahadori, Hemomediastinum and bilateral hemothorax with extensive angiomatosis of anterior mediastinum , Monaldi Archives for Chest Disease: Vol. 65 No. 3 (2006): Pulmonary series
- G.J. Wesseling, C.P. Van Schayck, Why act early in COPD? , Monaldi Archives for Chest Disease: Vol. 65 No. 3 (2006): Pulmonary series
- Furio Colivicchi, Francesco Fattirolli, Editors of Monaldi Archives for Chest Disease - Cardiac Series , Monaldi Archives for Chest Disease: Vol. 78 No. 1 (2012): Cardiac series
- Sabino Scardi, Le risorse della Cardiologia Riabilitativa , Monaldi Archives for Chest Disease: Vol. 66 No. 2 (2006): Cardiac series
- Giuseppe Caramia, Romualdo Belardinelli, Hyperhomocysteinemia in developing age and nutritional aspects of folates: an early cardiovascular risk factor , Monaldi Archives for Chest Disease: Vol. 66 No. 4 (2006): Cardiac series
- O. Serafini, G. Misuraca, A. Siniscalchi, M.T. Manes, G. Meringolo, C. Tomaselli, M. Chiatto, A. Buffon, Prevalence of aneurysm of the interatrial septum in the general population and in patients with a recent episode of cryptogenetic ischemic stroke: a tissue harmonic imaging transthoracic ecocardiography study in 5.631 patients , Monaldi Archives for Chest Disease: Vol. 66 No. 4 (2006): Cardiac series
- F.J. de Serres, I. Blanco, E. Fernández-Bustillo, PI S and PI Z Alpha-1 antitrypsin deficiency worldwide. A review of existing genetic epidemiological data , Monaldi Archives for Chest Disease: Vol. 67 No. 4 (2007): Pulmonary series
- Annamaria Municinó, Annamaria Nicolino, Manlio Milanese, Edoardo Gronda, Bruno Andreuzzi, Fabrizio Oliva, Francesco Chiarella, Hydrotherapy in Advanced Heart Failure: the Cardio-HKT Pilot Study , Monaldi Archives for Chest Disease: Vol. 66 No. 4 (2006): Cardiac series
- C. Carbonelli, S. Montepietra, A. Caruso, A. Cavazza, C. Feo, F. Menzella, L. Motti, L. Zucchi, Sarcoidosis and multiple sclerosis: systemic toxicity associated with the use of interferon-beta therapy , Monaldi Archives for Chest Disease: Vol. 77 No. 1 (2012): Pulmonary series
<< < 36 37 38 39 40 41 42 43 44 45 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/monaldi.2022.2151
https://doi.org/10.4081/monaldi.2022.2151





