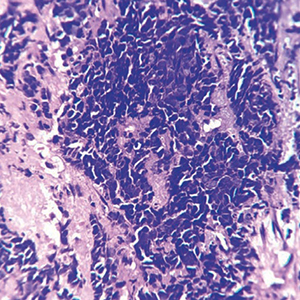
Detection of clinically-relevant EGFR variations in de novo small cell lung carcinoma by droplet digital PCR
Submitted: March 29, 2022
Accepted: August 2, 2022
Published: September 2, 2022
Accepted: August 2, 2022
Abstract Views: 1000
PDF: 406
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Ashok Kuwal, Manish Advani, Naveen Dutt, Seemant Saini, Surjit Singh, Diagnostic accuracy of semirigid thoracoscopy in exudative pleural effusions and relationship of thoracoscopic findings with probability of malignant diagnosis , Monaldi Archives for Chest Disease: Vol. 91 No. 3 (2021)
- Vidushi Rathi, Pranav Ish, Comments on “Mucoepidermoid carcinoma of the bronchus: a rare early diagnosis” , Monaldi Archives for Chest Disease: Early Access
- Cristiano Cesaro, Umberto Caterino, Fabio Perrotta, Umberto Masi, Alessandra Cotroneo, Roberta Cianci, Enzo Zamparelli, Flavio Cesaro, Dario Amore, Danilo Rocco, Alectinib rescue therapy in advanced ALK rearranged lung adenocarcinoma: a case report , Monaldi Archives for Chest Disease: Vol. 93 No. 3 (2023)
- E. Radzikowska, J. Pawlowski, M. Chabowski, R. Langfort, Constrictive bronchiolitis obliterans in patient with Castelman's disease , Monaldi Archives for Chest Disease: Vol. 63 No. 4 (2005): Pulmonary series
- Montserrat Diaz-Abad, Laura Malone, Liaqat Ali, Edward M. Pickering, Ashutosh Sachdeva, Acute eosinophilic pneumonia triggered by secondhand cigarette smoke exposure in an elderly man , Monaldi Archives for Chest Disease: Vol. 89 No. 1 (2019)
- Yuvarajan Sivagnaname, Praveen Radhakrishnan, Antonius Maria Selvam, Malignant bronchial ulcer with coexistent pulmonary tuberculosis , Monaldi Archives for Chest Disease: Vol. 89 No. 3 (2019)
- Igor S. Mamenko, Igor V. Vasilev, Irina A. Tabanakova, Sultan M. Gasanmagomedov, Vera V. Sysoeva, Alexey D. Ushkov, Tatiana A. Novickaya, Piotr K. Yablonskii, Probe-based confocal laser endomicroscopy in diagnosis of desquamative interstitial pneumonia in nonsmoker , Monaldi Archives for Chest Disease: Vol. 89 No. 3 (2019)
- Joana Vieira Naia, Diana Pimenta, Anita Paiva, Rita Costa, Conceição Souto de Moura, Raquel Pereira, João Filipe Cruz, When benign leiomyomas metastasize to the lungs - a case report , Monaldi Archives for Chest Disease: Vol. 93 No. 4 (2023)
- Igor Sergeevich Mamenko, Igor V. Vasilev, Roman V. Simonov, Anna S. Zakharova, Pavel V. Gavrilov, Ivetta V. Dvorakovskaya, Tatiana A. Novitskaya, Petr K. Yablonskiy, Probe-based confocal laser endomicroscopy in the diagnosis of diffuse cystic lung disease in Sjögren’s syndrome , Monaldi Archives for Chest Disease: Vol. 94 No. 3 (2024)
- Sotirios Kotoulas, Konstantinos Grapatsas, Charalampos Georgiou, Zoi Tsilogianni, Vasileios Leivaditis, Mariana Braga Lopes Rufino, Christophoros Kotoulas, Common swelling of the dorsal thoracic wall brings an unexpected finding: elastofibroma dorsi , Monaldi Archives for Chest Disease: Vol. 90 No. 1 (2020)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/monaldi.2022.2280
https://doi.org/10.4081/monaldi.2022.2280





