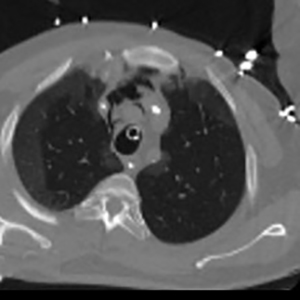
Pneumomediastinum in the COVID-19 era: to drain or not to drain?
Submitted: June 1, 2022
Accepted: July 20, 2022
Published: July 27, 2022
Accepted: July 20, 2022
Abstract Views: 1065
PDF: 326
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Annarita Pilleri, Giampaolo Scorcu, New assessment for advanced age: Italian study protocol on the assessment of surgical risk in the over-75-year age-group , Monaldi Archives for Chest Disease: Vol. 87 No. 2 (2017)
- Antonino Capizzi, Oliviero Sacco, Giovanni A. Rossi, Michela Silvestri, Recurrence of right lower lobe pneumonia 3 years after the first episode in an otherwise healthy 13-year-old girl , Monaldi Archives for Chest Disease: Vol. 87 No. 1 (2017)
- Alessandro Boccanelli, Pompilio Faggiano, Preoperative risk evaluation in patients over 75 years candidates to non-cardiac and cardiac surgery , Monaldi Archives for Chest Disease: Vol. 87 No. 2 (2017)
- Manas Pratim Roy, Risk factors for Covid-19 in India , Monaldi Archives for Chest Disease: Vol. 92 No. 2 (2022)
- Vijayarangam Narenchandra, Govindaraj Vishnukanth, Dharm Prakash Dwivedi, Munuswamy Hemachandren, Subathra Adithian, Saka Vinod Kumar, Manju Rajangam, Madhusmita Mohanty Mohapatra, Pratap Upadhya, Comparison of efficacy of autologous blood patch pleurodesis versus doxycycline pleurodesis in the management of persistent air leak in patients with secondary spontaneous pneumothorax. A randomized controlled trial , Monaldi Archives for Chest Disease: Vol. 92 No. 4 (2022)
- Yusuf Kayar, Nüket Bayram Kayar, Tuncay Şahutoğlu, Venkatanarayana Gangarapu, Spontaneous pneumomediastinum following pneumonia in a 23-year-old male patient , Monaldi Archives for Chest Disease: Vol. 83 No. 1-2 (2016): Pulmonary series
- Dario Amore, Emanuele Muto, Umberto Caterino, Dino Casazza, Alessandro Saglia, Pasquale Imitazione, Carlo Curcio, Anomalous segmental pulmonary vein: additional V6 behind the bronchus intermedius draining into the superior pulmonary vein , Monaldi Archives for Chest Disease: Vol. 92 No. 4 (2022)
- Nicola Rotolo, Maria Cattoni, Silvia De Maio, Luca Filipponi, Pau Mateo-Ramos, Andrea Imperatori, The surgical approach of late-onset tracheoesophageal fistula in a tracheostomized COVID-19 patient , Monaldi Archives for Chest Disease: Vol. 93 No. 4 (2023)
- Shivam Garg, Vishnukanth Govindaraj, Dharm Prakash Dwivedi, Kalayarasan Raja, Elamurugan Palanivel Theerthar, Postoperative pulmonary complications in patients undergoing upper abdominal surgery: risk factors and predictive models , Monaldi Archives for Chest Disease: Early Access
- Francesco Barillà , Concetta Torromeo, Riccardo Iorio, Luigina Porco, Vincenzo Paravati, Carlo Gaudio, Antiplatelet therapy in elderly patients with acute coronary syndrome: Between scientific evidence and future perspectives , Monaldi Archives for Chest Disease: Vol. 88 No. 2 (2018)
<< < 5 6 7 8 9 10 11 12 13 14 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/monaldi.2022.2338
https://doi.org/10.4081/monaldi.2022.2338





