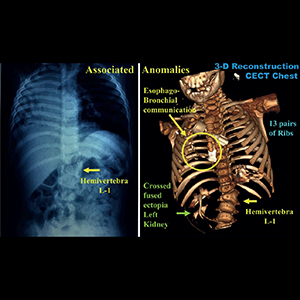
Bronchiectasis without lower respiratory symptoms in the presence of multisystem anomalies – a clinical clue to diagnose esophageal lung anomaly
Submitted: June 2, 2022
Accepted: June 27, 2022
Published: July 4, 2022
Accepted: June 27, 2022
Abstract Views: 704
PDF: 187
Video: 97
Video: 97
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- Martina Turrin, Francesca Maria Pontoriero, Giulia Grisostomi, Giordano Fiorentù, Francesca Zampieri, Francesca Savoia, Cosimo Catino, Giuseppe Zanardi, Piera Peditto, Nicola Malacchini, Fabiola Zeraj, Matteo Bonato, Diana Sacchi, Maria Guido, Giovanni Morana, Micaela Romagnoli, Tracheal atypical solitary carcinoid in a so-called “difficult asthma”: a diagnostic challenge , Monaldi Archives for Chest Disease: Vol. 94 No. 2 (2024)
- Vinh Nguyen-Nhu, Lam-Phuoc Nguyen, Sy Duong-Quy, Pham Le An, Tri Bui-Minh, Classification of chronic obstructive pulmonary disease as ABCD according to the GOLD 2011 and 2017 versions in patients at the University Medical Center in Ho Chi Minh City, Vietnam , Monaldi Archives for Chest Disease: Vol. 94 No. 2 (2024)
- Raffaele Martone, Niccolò Marchionni, Francesco Cappelli, Heart failure with mid-range ejection fraction: Current evidence and uncertainties , Monaldi Archives for Chest Disease: Vol. 89 No. 1 (2019)
- Rafael Martínez-Girón, Liron Pantanowitz, Pulmonary actinomycosis: cytomorphological features , Monaldi Archives for Chest Disease: Vol. 92 No. 2 (2022)
- Dario Amore, Dino Casazza, Alessandro Saglia, Pasquale Imitazione, Umberto Caterino, Carlo Curcio, How to avoid "en masse" lobectomy using VATS technique in presence of hilar fibrosis , Monaldi Archives for Chest Disease: Vol. 91 No. 2 (2021)
- Devendra Kumar Singh, Gaurav Pandey, Syed Haider Mehdi Rizvi, Pankaj Kumar Singh, Isolated pulmonary hemorrhage after electric shock: a rare phenomenon , Monaldi Archives for Chest Disease: Vol. 94 No. 1 (2024)
- Joana Almeida Borges, Antonio M. Esquinas, Biphasic cuirass ventilation in the escalation of non-invasive ventilation in COVID-19: Case report and review , Monaldi Archives for Chest Disease: Vol. 93 No. 4 (2023)
- Natalia Adamashvili, Kristina Akopyan, Nestani Tukvadze, Kostyantyn Dumchev, Yuliia Sereda, Irma Khonelidze, Giorgi Kuchukhidze, Factors associated with loss to follow-up among people with tuberculosis in the country of Georgia: a cohort study , Monaldi Archives for Chest Disease: Vol. 91 No. 1 (2021)
- Christos Kakos, Savvas Lampridis, Georgios Geropoulos, Reena Khiroya, Achilleas Antonopoulos, Sofoklis Mitsos, Nikolaos Panagiotopoulos, The challenging management of a giant intrathoracic desmoid tumour: a case report , Monaldi Archives for Chest Disease: Vol. 91 No. 3 (2021)
- Emanuele Stirpe, Floriana Bardaro, Johanna Köhl, Intracavitary fibrinolysis directly under vision during medical thoracoscopy: a case report , Monaldi Archives for Chest Disease: Vol. 93 No. 3 (2023)
<< < 31 32 33 34 35 36 37 > >>
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/monaldi.2022.2342
https://doi.org/10.4081/monaldi.2022.2342





