Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.
Chest ultrasound findings in usual interstitial pneumonia patterns: a pilot study
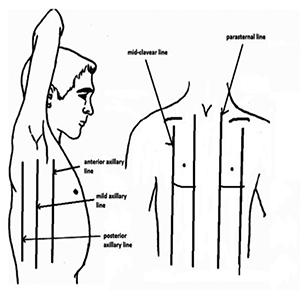
It is unknown what role chest ultrasound plays in distinguishing the various usual interstitial pneumonia (UIP) patterns of high-resolution chest tomography (HRCT). The purpose of this study was to see if there was a link between the results of chest ultrasound (u/s) and HRCT in patients with idiopathic pulmonary fibrosis (IPF). We performed chest u/s in 16 patients with UIP and probable UIP patterns to indeterminate UIP and alternative diagnosis patterns in this single center prospective study to determine any possible relationship with the HRCT findings. A chest radiologist reviewed each HRCT to determine the pattern in accordance with the American Thoracic Society (ATS) / European Respiratory Society (ERS) Guidelines. The local multidisciplinary committee validated the patients' diagnoses before they were included. When compared to the indeterminate for UIP or alternative diagnosis pattern group, there was a trend (p=0.07) toward the presence of more B lines in UIP or probable UIP patterns. There was no statistically significant difference in the presence of small, large, white lung, or pleural line thickening >5mm. Subgroup analysis revealed that patients with honeycombing were more likely to have a fragmented pleural line (p=0.04). To summarize, in our pilot study, chest u/s appears unable to differentiate UIP and probable UIP patterns from indeterminate UIP and alternative diagnosis patterns. However, it appears that this technique can be used to recognize the honeycombing pattern.
Ethics Approval
This study was approved by the Internal Review Board of the University Hospital of Saint Etienne, France (IRBN462019/CHUSTE)How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/monaldi.2022.2356
https://doi.org/10.4081/monaldi.2022.2356