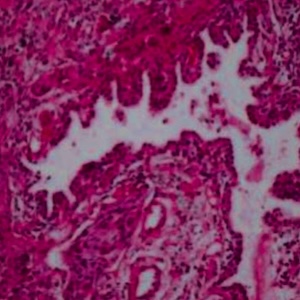
Subtyping of advanced lung cancer based on PD-L1 expression, tumor histopathology and mutation burden (EGFR and KRAS): a study from North India
Submitted: October 4, 2022
Accepted: December 13, 2022
Published: February 1, 2023
Accepted: December 13, 2022
Abstract Views: 1286
PDF: 330
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Similar Articles
- T. Kontakiotis, N. Manolakoglou, F. Zoglopitis, D. Iakovidis, L. Sacas, A. Papagiannis, A. Mandrali, D. Papakosta, P. Argyropoulou, D. Bouros, Epidemiologic trends in lung cancer over two decades in Northern Greece: an analysis of bronchoscopic data , Monaldi Archives for Chest Disease: Vol. 71 No. 4 (2009): Pulmonary series
- Amanda R. Jimenez, Arielle Shaeffer Weiss, Anthony C. Campagna, Use of pulmonary function test demographic data to identify high-risk patients for lung cancer screening , Monaldi Archives for Chest Disease: Vol. 88 No. 1 (2018)
- Janet Fallon, Martin Plummeridge, Richard Daly, Andrew Medford, Linear probe 19-gauge endobronchial ultrasound diagnosis of a benign chondroid hamartoma , Monaldi Archives for Chest Disease: Vol. 88 No. 1 (2018)
- P. Pirina, M. Budroni, S. Esposito, S. Ostera, M.F. Polo, L. Santoru, G. Madeddu, A.G. Fois, G.C. Ginesu, G. Padua, F. Tanda, F. Ginesu, Cytological and histological diagnosis of lung cancer in Sardinia and Italy in the 1990s , Monaldi Archives for Chest Disease: Vol. 67 No. 4 (2007): Pulmonary series
- G.L. Casoni, C. Gurioli, P.N. Chhajed, M. Chilosi, M. Zompatori, D. Olivieri, V. Poletti, The value of transbronchial lung biopsy using jumbo forceps via rigid bronchoscope in diffuse lung disease , Monaldi Archives for Chest Disease: Vol. 69 No. 2 (2008): Pulmonary series
- Vishal Chopra, Hardik Jain, Akhil D. Goel, Siddharth Chopra, Ashrafjit S. Chahal, Neha Garg, Vidhu Mittal, Correlation of aspergillus skin hypersensitivity with the duration and severity of asthma , Monaldi Archives for Chest Disease: Vol. 87 No. 3 (2017)
- H. Halilcolar, S. Yapicioglu, S. Bilaceroglu, Temporal Changes in Lung Cancer: A 10-year Study in a Chest Hospital , Monaldi Archives for Chest Disease: Vol. 69 No. 4 (2008): Pulmonary series
- Emanuela Barisione, Carlo Genova, Marco Grosso, Mercedes Pasquali, Alessandro Blanco, Raffaella Felletti, Mario Salio, Palliative treatment of life-threatening hemoptysis with silicone stent insertion in advanced lung cancer , Monaldi Archives for Chest Disease: Vol. 87 No. 1 (2017)
- Ali Asghar Hemmati, Soheila Alboghobeish, Akram Ahangarpour, Chronic exposure to high fat diet exacerbates arsenic-induced lung damages in male mice: Possible role for oxidative stress , Monaldi Archives for Chest Disease: Vol. 88 No. 1 (2018)
- Rajesh Venkataram, Srividya Arjuna, Giridhar Belur Hosmane, Anirban Chakraborty, Quantitative analysis of cell-free DNA by droplet digital PCR reveals the presence of EGFR mutations in non-malignant lung pathologies , Monaldi Archives for Chest Disease: Vol. 91 No. 3 (2021)
You may also start an advanced similarity search for this article.

 https://doi.org/10.4081/monaldi.2023.2449
https://doi.org/10.4081/monaldi.2023.2449





